FLS BENEFITS
Fracture Liaison Service (FLS) – Secondary Fracture Prevention
The Fracture Liaison Service (FLS) secondary fracture prevention program coordinated care model has been in operation for more than 15 years in the United States and other countries to close the secondary fracture prevention care gap. They ensure that patients suffering fractures caused by osteoporosis undergo a fracture risk assessment to prevent further fractures by treatment of osteoporosis and falls prevention strategies, delivering highly effective care while significantly reducing the costs associated with secondary fractures.
A narrative review published in Osteoporosis International in early 2017 summarized the efficacy of a range of osteoporosis treatments in the secondary prevention of fragility fractures. Several randomized controlled trials (RCTs) have demonstrated the effectiveness of treatment of individuals with low bone mass who have prevalent vertebral fractures.
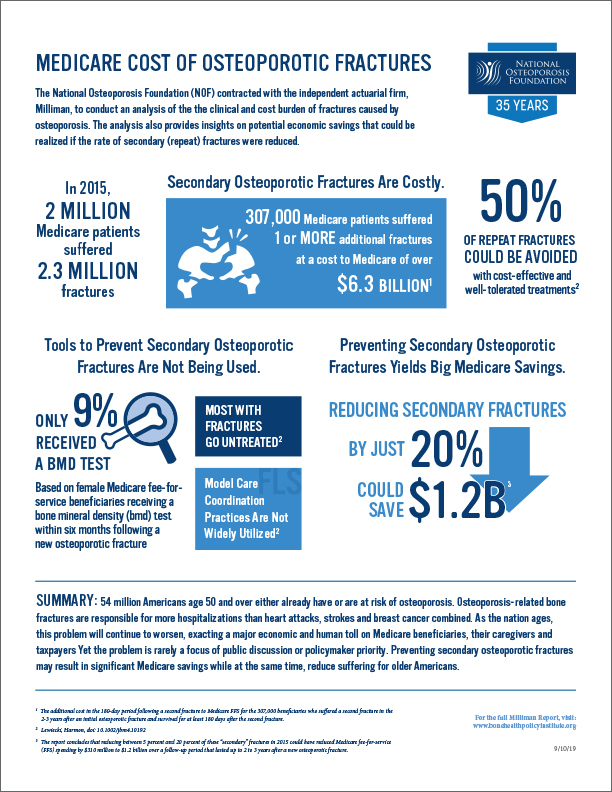
Hansen, D, Bazell C, Pelizzari P, Pyenson B. Medicare cost of osteoporotic fractures. https://www.milliman.com/insight/2019/Medicare-cost-of-osteoporotic-fractures/. Published 2019. Accessed September 18, 2019.
The overwhelming majority (>80%) of individuals with fragility fractures at all skeletal sites are neither assessed for osteoporosis nor offered treatment. Given that rates of diagnosis and recognition of vertebral fractures are considerably lower than for non-vertebral fractures, it is likely that the care gap is even greater for individuals with vertebral fractures.
Fracture Liaison Services (FLS) are models of care devised to ensure that individuals who sustain fragility fractures receive osteoporosis assessment and are referred for falls interventions, where appropriate. Strategies to improve vertebral fracture case finding include introduction of vertebral fracture assessment (VFA) into FLS protocols and engagement with colleagues in radiology to develop a systematic approach to opportunistic identification of vertebral fractures among older individuals undergoing routine chest radiographs, CT and MRI scans.
A FLS program operates under the supervision of osteoporosis specialists and collaborates with the patient’s primary care physician. Usually led by nurse practitioners or other allied health professionals, it ensures older adult fracture patients receive appropriate diagnosis and treatment of their likely osteoporosis. The program creates a population registry of fracture patients and establishes a process and timeline for patient assessment and follow-up care. In addition to managing osteoporosis, where appropriate, FLS programs will refer patients to falls prevention services. The distinguishing feature of the co-care model, compared to traditional models of care, is that the orthopedic surgeon and the geriatrician share the responsibility of care and the patient is managed by an interdisciplinary team. In the United States, the co-care model has been referred to as a Geriatric Fracture Center (GFC).